Author:
Dr. med. Walter Hugentobler
Specialist in general internal medicine
Dr. med. Walter Hugentobler
Specialist in general internal medicine
The Coronavirus causes flu symptoms such as coughing or difficulty breathing.
Inactivation of SARS coronavirus surrogate TGEV after 2 days
Inactivation of SARS coronavirus surrogate TGEV outdoors
Dr. med. Walter Hugentobler / FMH General and Internal Medicine
The Chinese health authorities have promptly reported new illnesses and deaths and are working closely with the WHO. The drastic travel restrictions, which now affect more than 50 million people, prove that the situation is classified as very serious. These extremely drastic measures are unprecedented in the recent history of fighting epidemics and pandemics. Their effects and possible side effects cannot currently be assessed.
The new corona virus 2019-nCoV, whose genetic code has already been deciphered and communicated openly, is closely related to the SARS virus. Laboratories worldwide have been able to use this information to develop tests for virus detection. The virus is said to have been transmitted to humans at an open meat market in Wuhan, which also offers live wild animals, and is now spreading from person to person. It causes flu symptoms, such as coughing and difficulty breathing, in some of the people affected. X-rays show an untreatable pneumonia that can lead to death. What is worrying is that in comparison with the current epidemic with the SARS pandemic 2002/2003, both the temporal and the spatial spread in the current case are much faster.
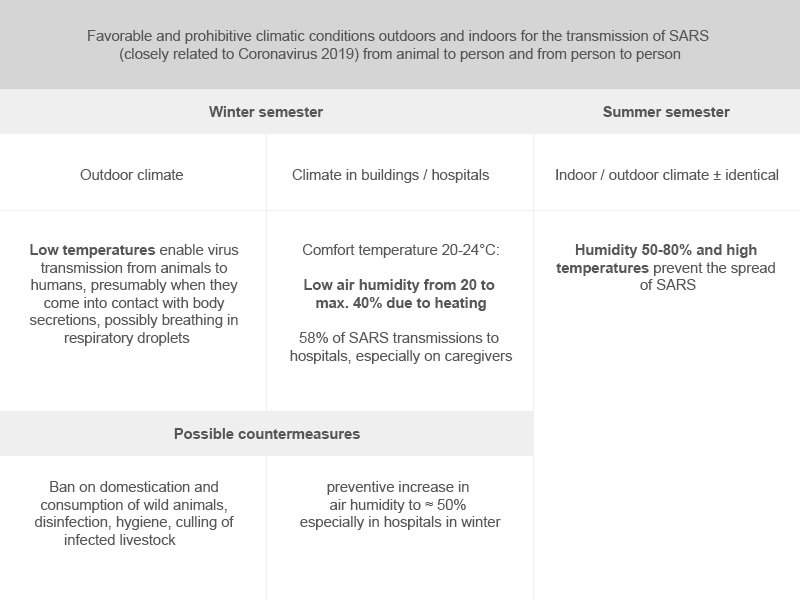
The combination of research results on the resistance of coronaviruses to humidity and temperature with data on the SARS pandemic and the MERS epidemic (both caused by variants of the coronavirus) now yields interesting new insights. Both the crossing of the animal-human species boundary and the transmission from human to human are obviously made possible or respectively blocked by typical combinations of humidity and air temperature. It is known that coronaviruses can spread primarily within wild mammals and birds. These animals are also domesticated in China and sold live in open market halls for purchase and subsequent consumption.
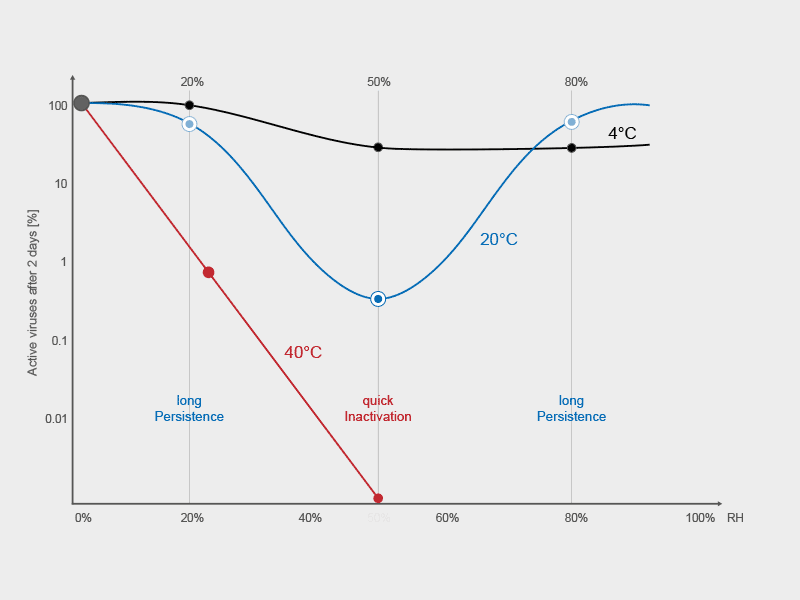
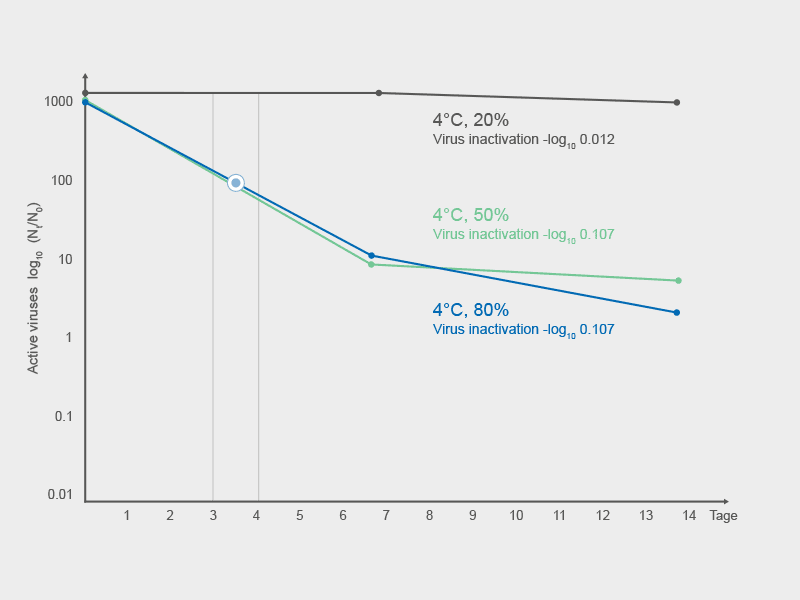
The survival times of SARS and MERS corona viruses on inanimate surfaces and as infectious droplets in the air have been examined several times and extensively. An identical pattern was repeatedly shown. Very low temperatures and humidity enable the viruses to survive on surfaces and in the air for a long time. The survival time was long even at medium temperatures of 20 to 30°C - but only when the air was dry. Very high temperatures (> 30°C) inactivate the corona viruses. This is why the repeated MERS epidemics in the Arabian Peninsula only occurred in the cooler winter months. It is to be expected that the current Corona Virus 2019 will exhibit a similar behavior towards humidity and temperature.
The crossing of the species boundary must take place outdoors, where infectious animals are and humans come into contact with them. The spread of the virus from person to person takes place, however, where people are mostly (approx. 90% of their lifetime) and maintain their contacts, i.e. practically exclusively in buildings and on public transport. It must be borne in mind that the indoor and outdoor climates differ significantly when heating occurs in the buildings due to the low outside temperatures. The result is comfort temperatures of 20 to 24 °C combined with unnaturally low humidity.
Why is the transmission situation in central and southern China ideal for corona viruses in the winter months? (see table).
In wintery China, the open market halls for meat sales have optimal low temperatures for animal-to-human transmission. As already stated, the indoor conditions are decisive for the transmission conditions from person to person. In central and southern China, the winter outside temperatures are in an area that requires heating the houses. The temperatures in the houses and public transport are between 20 and 24 degrees and the humidity in the heated rooms at a low 20 to a maximum of 40%. These are ideal climatic conditions for the long survival of SARS corona viruses on surfaces and in the air and thus also for the transmission through contacts and via the air.
The outdoor climatic situation, which enables the species boundary to be crossed, cannot be influenced by humans. But he is responsible for the indoor climate. The decisive factors temperature, humidity, air exchange rate and fresh air percentage can be individually controlled. Since the comfort temperature is set at 20 to 24 °C, the risk of infection in buildings must be influenced by the air humidity and ventilation. An increase in the low air humidity in the buildings by humidification to around 50% leads to a reduction in the transmission risk. The increase in the air exchange rate and an increased fresh air percentage result in an additional risk reduction.
Air humidification also has a proactive effect against the spread of viruses by the sick, including so-called "super spreaders", before symptoms appear or a diagnosis can be made. In addition, the humidified air improves the defense situation of the airways in healthy people, through more efficient cleaning of the airways and improved immune defense. The preventive increase in the too low humidity in the buildings in winter is a cost-effective and effective tool for reducing the risk of spreading without causing side effects. Since around 58% of SARS cases occurred as a result of hospital broadcasts, humidification in hospitals is expected to have a disproportionately large, positive effect. Humidification can also be used in public buildings and in private and professional environments. Humidification provides the population with a simple means of actively combating the current virus, against which there is currently no vaccine or specific medication.
Scientific study "Effects of Air Temperature and Relative Humidity on Coronavirus Survival on Surfaces"
This study clearly shows that maintaining average humidity in hospitals and healthcare facilities would be an effective measure to reduce the risk of coronavirus transmission.
Although this study is intended to provide an insight into possible measures to combat SARS-CoV (the virus of the SARS pandemic in 2002/2003), the results are most likely for the spread of COVID-19, that of SARS-CoV-2 transmitted disease, relevant, a coronavirus that is genetically very close to SARS-CoV.
Regulators and hospital designers need to be aware of the available scientific evidence, such as this study, and focus more on moisture control as a common infection control measure.

 In heated, dry rooms (20°C, 20% RH) in winter ≈ 80% of corona viruses on surfaces are still infectious after one week. They can be transmitted from there to people by direct and indirect contact or by being whirled up in the air.
In heated, dry rooms (20°C, 20% RH) in winter ≈ 80% of corona viruses on surfaces are still infectious after one week. They can be transmitted from there to people by direct and indirect contact or by being whirled up in the air.

 If the air is humidified to 50%, less than 1% of the viruses are still infectious after 2 days. This considerably reduces the risk of transmission.
If the air is humidified to 50%, less than 1% of the viruses are still infectious after 2 days. This considerably reduces the risk of transmission.

In addition to the current pandemic measures, additional humidification with a focus on hospitals could further reduce the risk of spreading Coronavirus 2019.
The Chinese health authorities have promptly reported new illnesses and deaths and are working closely with the WHO. The drastic travel restrictions, which now affect more than 50 million people, prove that the situation is classified as very serious. These extremely drastic measures are unprecedented in the recent history of fighting epidemics and pandemics. Their effects and possible side effects cannot currently be assessed.
The new corona virus 2019-nCoV, whose genetic code has already been deciphered and communicated openly, is closely related to the SARS virus. Laboratories worldwide have been able to use this information to develop tests for virus detection. The virus is said to have been transmitted to humans at an open meat market in Wuhan, which also offers live wild animals, and is now spreading from person to person. It causes flu symptoms, such as coughing and difficulty breathing, in some of the people affected. X-rays show an untreatable pneumonia that can lead to death. What is worrying is that in comparison with the current epidemic with the SARS pandemic 2002/2003, both the temporal and the spatial spread in the current case are much faster.
The combination of research results on the resistance of coronaviruses to humidity and temperature with data on the SARS pandemic and the MERS epidemic (both caused by variants of the coronavirus) now yields interesting new insights. Both the crossing of the animal-human species boundary and the transmission from human to human are obviously made possible or respectively blocked by typical combinations of humidity and air temperature. It is known that coronaviruses can spread primarily within wild mammals and birds. These animals are also domesticated in China and sold live in open market halls for purchase and subsequent consumption.
The survival times of SARS and MERS corona viruses on inanimate surfaces and as infectious droplets in the air have been examined several times and extensively. An identical pattern was repeatedly shown. Very low temperatures and humidity enable the viruses to survive on surfaces and in the air for a long time. The survival time was long even at medium temperatures of 20 to 30°C - but only when the air was dry. Very high temperatures (> 30°C) inactivate the corona viruses. This is why the repeated MERS epidemics in the Arabian Peninsula only occurred in the cooler winter months. It is to be expected that the current Corona Virus 2019 will exhibit a similar behavior towards humidity and temperature.
The crossing of the species boundary must take place outdoors, where infectious animals are and humans come into contact with them. The spread of the virus from person to person takes place, however, where people are mostly (approx. 90% of their lifetime) and maintain their contacts, i.e. practically exclusively in buildings and on public transport. It must be borne in mind that the indoor and outdoor climates differ significantly when heating occurs in the buildings due to the low outside temperatures. The result is comfort temperatures of 20 to 24 °C combined with unnaturally low humidity.
Why is the transmission situation in central and southern China ideal for corona viruses in the winter months? (see table).
In wintery China, the open market halls for meat sales have optimal low temperatures for animal-to-human transmission. As already stated, the indoor conditions are decisive for the transmission conditions from person to person. In central and southern China, the winter outside temperatures are in an area that requires heating the houses. The temperatures in the houses and public transport are between 20 and 24 degrees and the humidity in the heated rooms at a low 20 to a maximum of 40%. These are ideal climatic conditions for the long survival of SARS corona viruses on surfaces and in the air and thus also for the transmission through contacts and via the air.
The outdoor climatic situation, which enables the species boundary to be crossed, cannot be influenced by humans. But he is responsible for the indoor climate. The decisive factors temperature, humidity, air exchange rate and fresh air percentage can be individually controlled. Since the comfort temperature is set at 20 to 24 °C, the risk of infection in buildings must be influenced by the air humidity and ventilation. An increase in the low air humidity in the buildings by humidification to around 50% leads to a reduction in the transmission risk. The increase in the air exchange rate and an increased fresh air percentage result in an additional risk reduction.
Air humidification also has a proactive effect against the spread of viruses by the sick, including so-called "super spreaders", before symptoms appear or a diagnosis can be made. In addition, the humidified air improves the defense situation of the airways in healthy people, through more efficient cleaning of the airways and improved immune defense. The preventive increase in the too low humidity in the buildings in winter is a cost-effective and effective tool for reducing the risk of spreading without causing side effects. Since around 58% of SARS cases occurred as a result of hospital broadcasts, humidification in hospitals is expected to have a disproportionately large, positive effect. Humidification can also be used in public buildings and in private and professional environments. Humidification provides the population with a simple means of actively combating the current virus, against which there is currently no vaccine or specific medication.
Scientific study "Effects of Air Temperature and Relative Humidity on Coronavirus Survival on Surfaces"
This study clearly shows that maintaining average humidity in hospitals and healthcare facilities would be an effective measure to reduce the risk of coronavirus transmission.
Although this study is intended to provide an insight into possible measures to combat SARS-CoV (the virus of the SARS pandemic in 2002/2003), the results are most likely for the spread of COVID-19, that of SARS-CoV-2 transmitted disease, relevant, a coronavirus that is genetically very close to SARS-CoV.
Regulators and hospital designers need to be aware of the available scientific evidence, such as this study, and focus more on moisture control as a common infection control measure.
Inactivation of SARS coronavirus surrogate TGEV
The indoor climate, where we spend 90% of our lives, is decisive for the transmission of the viruses from person to person. This is where most of the human-to-human contact takes place and this is where we share the available indoor air.
The indoor climate, where we spend 90% of our lives, is decisive for the transmission of the viruses from person to person. This is where most of the human-to-human contact takes place and this is where we share the available indoor air.
Inactivation of SARS coronavirus surrogate TGEV at room temperature 20°C and at different Room air humidity of 20% (Fig. 1), 50% (Fig. 2) and 80% (Fig. 3). Fastest inactivation at 50% RH (- 2.5 log10 in 2 days).
Interactive map of John Hopkins University